This is the third installment of a three-part series highlighting the need for improved efficiencies in hospitals and outpatient care clinics. Part 1 examines capital considerations and the pursuit of decarbonization. Part 2 addresses technological challenges, space constraints and staffing demands.
With calls to improve patient care, operational efficiency, sustainability, and financial performance, healthcare facilities managers get pulled in numerous directions at once. How can they make progress when facing so many competing demands? A trio of priorities must take center stage, experts say — technology, sustainability and benchmarking — with the three working together to result in more efficient and cost-effective operations.
More technology and technological upskilling
Ernst and Young Managing Director Richard Taylor has created facilities knowledge centers in multiple healthcare organizations.

In an interview, he listed three steps that facilities leaders can take to accelerate their digital upskilling efforts. The first step involves understanding the need for technological applications that can provide the data required for improved patient convenience. The second is knowing how much capital is needed to invest in AI-powered tools and equipment that can provide reliable data points. The third is training facilities teams on the analytics to obtain insight into those data points.
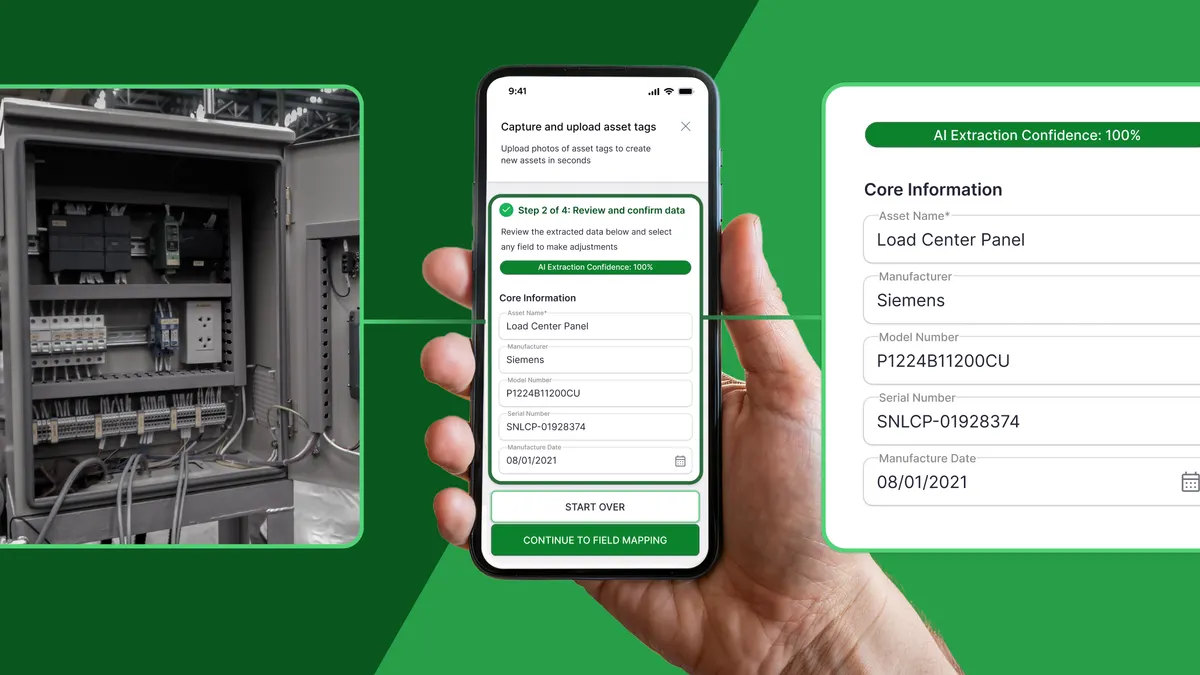
“Hospitals and outpatient facilities are using automation to improve experience, all the way from installing sensors in soap dispensers to more sophisticated aspects like monitoring air pressure in operating theaters,” he said.
An automation-driven “patient experience” approach is also more likely to draw younger patients back to first-time medical specialists for subsequent visits. JLL recently reported on a growing preference for additional healthcare amenities among younger generations as a driver of positive experience during first-time visits. The findings of JLL’s 2023 Patient Consumer Survey suggest that patients and guests of healthcare facilities, particularly those in urban areas, struggle with long wait times in overcrowded areas and difficulties with wayfinding or landing a parking spot.
“People are using apps on their iPhones to find their way around a facility,” Taylor said. “Most health systems these days understand that it’s a more consumer-driven world today, even in healthcare. And that translates to facilities managers.”
A sustainability mindset
Mark Grinis, who leads digital transformation initiatives for EY Americas’ real estate business, points to the need for building management systems, equipped with smart technology, that can turn lights off in empty rooms and adjust temperatures based on usage. “It’s critical to understand how the building is being used and then modulate energy consumption,” he said.
As system leader for facilities management and construction at Trinity Health, Andy Woommavovah is looking to upgrade fluorescent lighting to LED systems across facilities in certain locations. He is also working to replace aged chillers and refrigerants with energy-efficient ones. He said building automation systems and remote fault detection make it easier to replace outdated pieces of equipment with modern ones that consume less energy and do not contribute as much to emissions.
“The whole technology piece is going to be a game changer if we can afford to overlay that investment into our work because it allows us to remotely monitor hundreds of assets, and ensure they are operating within set parameters while also helping us detect malfunctions and failures,” he said.
Robert Melton, who manages 75 facilities workers for Cape Fear Valley Health Systems as the corporate director of engineering, believes sustainability is more of an opportunity for healthcare facilities managers than a hindrance. “We have to decarbonize as much as possible to decrease carbon footprint and reduce energy costs,” he said. “We are not seeing it as a stumbling block. We are addressing it, and I think it’s the right thing to do.”
But many facilities managers in the space are struggling to get started. Although certain healthcare systems that initiated decarbonization efforts before COVID-19 are faring well, a majority of those that did not are trying to figure out ways to decarbonize in a vacuum of post-pandemic financial stringency, Woommavovah noted.
Energy Star, a program managed by the U.S. Environmental Protection Agency, offers the Portfolio Manager energy use benchmarking tool, which healthcare facilities managers can use to improve their sustainability efforts.
“It's free to use,” said Jennifer Leitsch, managing director of climate change and sustainability services at EY. “You set up an account and put in some basic information about your building, like the building size, occupancy, what it's used for, etc. And then you can connect directly to your utility, and you can have them feed data into the Energy Star Portfolio Manager tool.”
The tool provides a score indicating your building’s energy performance relative to similar buildings in the U.S., considering factors such as energy usage per square foot per year, climate, location, imaging equipment and the number of staffed beds, according to a primer from the Agency for Healthcare Research and Quality. For instance, an Energy Star score of 75 indicates that the building is in the top 75th percentile for performers among nationwide buildings that have the same primary use.
Budget management and benchmarking
Given the labor scarcity and resource crunch, facilities managers are working harder to boost net revenue and cash flow.
Melton said facilities managers need to prioritize benchmarking to find operating efficiencies and cost optimization. “You may have certain teams, like administrative staff, shut down by 5 [p.m.] or 6 p.m. A hospital with 2,000 employees may have teams working in shifts,” he said, noting that facilities leads need to determine how energy costs can be reduced in those spaces.
“We’d love to have more capital to do more projects,” he added, emphasizing that since a bulk of existing budgets is spent on salaries, it becomes crucial to clearly determine and allocate expenses and anticipated investments in non-labor activities like repairs, upgrades and preventive maintenance.
The vast size of most provider networks increases the complexity of facility planning and maintenance, especially in the face of a need for continuous improvements, new construction projects and renovations to improve patient care and remain competitive, according to Mark Kenneday, director of market strategy and development for healthcare at Gordian.
Modern Healthcare recently reported Kenneday’s emphasis on the importance of facility condition assessments in easing facility planning decisions and driving value in healthcare organizations. “The result is a verified, accurate and reliable inventory of an organization’s facilities infrastructure, including all physical assets that require funding to maintain,” Kenneday told Modern Healthcare.

Alison Flynn Gaffney, who leads JLL’s healthcare division, emphasizes the importance for healthcare companies to recognize and elevate facilities managers as strategic partners. “I believe that will continue to grow at scale,” she said. “Investing in facilities managers creates [an] enhanced patient safety and caregiver experience. It’s a competitive advantage for systems that truly recognize the value of facilities managers.''